Sudden cardiac death SCD ends the lives of many people every year and it does so unpredictably. In North America and Europe cases reach 50-100 per 100,000 per year and the most common cause is due to ventricular arrhythmias. It is difficult to carry out risk assessment with those who have hypertrophic cardiomyopathy (HCM) which is common- inherited heart disease, 1 in 200-500 people. HCM makes the wall of the heart thick, predisposing it to SCD, particularly among adults.
The existing recommendations, such as the ones developed by the ACC/AHA and ESC are incomplete. They depend on such factors as low ejection fraction, yet most patients with HCM have richly functional hearts and still are under risks. In comes MAARS (Multimodal Artificial Intelligence for Ventricular Arrhythmia Risk Stratification), a potentially revolutionary AI technology developed by Johns Hopkins and partners. Published in the Nature Cardiovascular Research, MAARS harnesses deep learning to foresee life-threatening arrhythmias thus possibly saving a life.
The Science of how MAARS Works: Multimodal Data
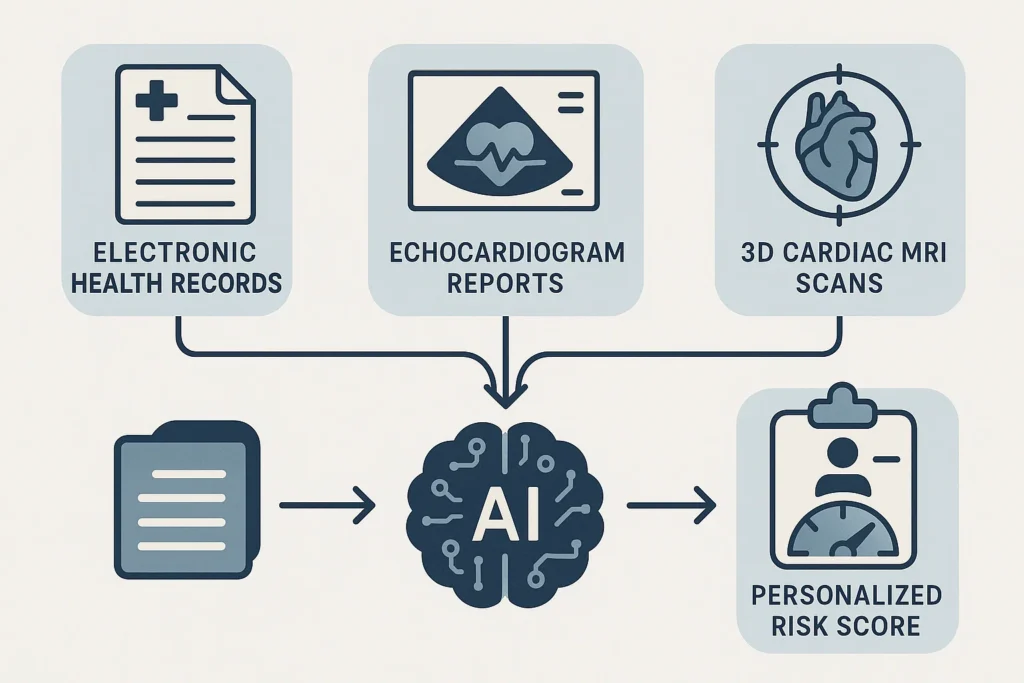
MAARS is not the usual predictor: it is a neural network of a transformer that reads using different data:
Electronic Health Records (EHRs): demographics, medical history, symptoms.
Imaging Reports: echocardiograms, CMR facts on cardiac structure.
Contrast-Enhanced CMR Images: Raw scans of CMR revealing fibrosis, which is a primary cause of arrhythmia.
Each modality is processed by three special branches, including a 3D Vision Transformer for CMR images (retains the spatial information), and feedforward networks of EHRs /reports. A multimodal fusion chapter pools together insights to derive personalised risk scores.
This arrangement apes the way physicians incorporate data albeit at the speed and accuracy rate of AI. MAARS does not have the same issues as guidelines, which is complicated patterns in raw data that could produce a bias by being interpreted manually.
Superior outcomes: Beating Clinical Baselines
Tested on 553 Johns Hopkins patients (internal) and 286 from Sanger Heart & Vascular Institute (external), MAARS shone:
Internal Validation: AUC of 0.89, balanced accuracy 0.80—beating guidelines’ 0.54-0.62 by 0.27-0.35.
External Validation: AUC 0.81, improvements of 0.22-0.30 over guidelines.
It forecasted SCD due to arrhythmia (e.g., ventricular tachycardia/fibrillation) with great sensitivity/specificity. This was in contrast to biased guidelines because fairness checks displayed consistent performance irrespective of sex and age.
Ablation studies supported the idea that multimodal fusion increases accuracy: single-modality variants were lower. Such features of interpretability as attention maps identify the most important factors: the degree of fibrosis, family history of SCD, non sustained ventricular tachycardia.
Why It Matters: Closing Care Gaps in HCM
HCM is heterogeneous; risk stratification is challenging- guidelines result in miss-protections or unnecessary ICDs. MAARS would have an opportunity to optimize decisions, minimizing overtreatment (a lot of ICDs are not used) and covering serious cases.
The advantage of MAARS might forestall tragedies with the percentage of internal and external patients who suffered an event being 19/553 and 25/286 compared. It is openly observed: model interpretations can be transparent, as they provide clues into the subject of study, such as the role of CMR fibrosis.
Limitations? Cohorts are U.S based; general validation is required. Missing data has been imputed but gaps exist in the real-world. AI applications require monitoring.
Clinical Impact & Future Potential
If integrated into everyday practice, MAARS could:
Reduce preventable deaths by identifying high-risk patients earlier
Avoid unnecessary ICD procedures, lowering costs and patient risk
Support precision medicine by tailoring prevention strategies to each individual
While the study’s relatively small patient numbers mean more validation is needed, the model’s ability to work across different hospital systems is promising.
Conclusion: A life-saving discovery
The development of MAARS marks a major leap forward in cardiovascular AI. By fusing MRI scans, medical histories, and echocardiogram data, it delivers personalized, accurate, and fair risk predictions for one of the most complex challenges in cardiology: sudden cardiac death in hypertrophic cardiomyopathy.
With further validation, this multimodal AI could help doctors save lives by ensuring that the right patients get the right protection at the right time.
References & Resources
Lai, C., et al. (2025). Multimodal AI to forecast arrhythmic death in hypertrophic cardiomyopathy. Nature Cardiovascular Research, 4, 891–903. https://doi.org/10.1038/s44161-025-00679-1
American College of Cardiology (ACC) & American Heart Association (AHA) Guidelines for HCM.
European Society of Cardiology (ESC) Guidelines for Cardiomyopathies.