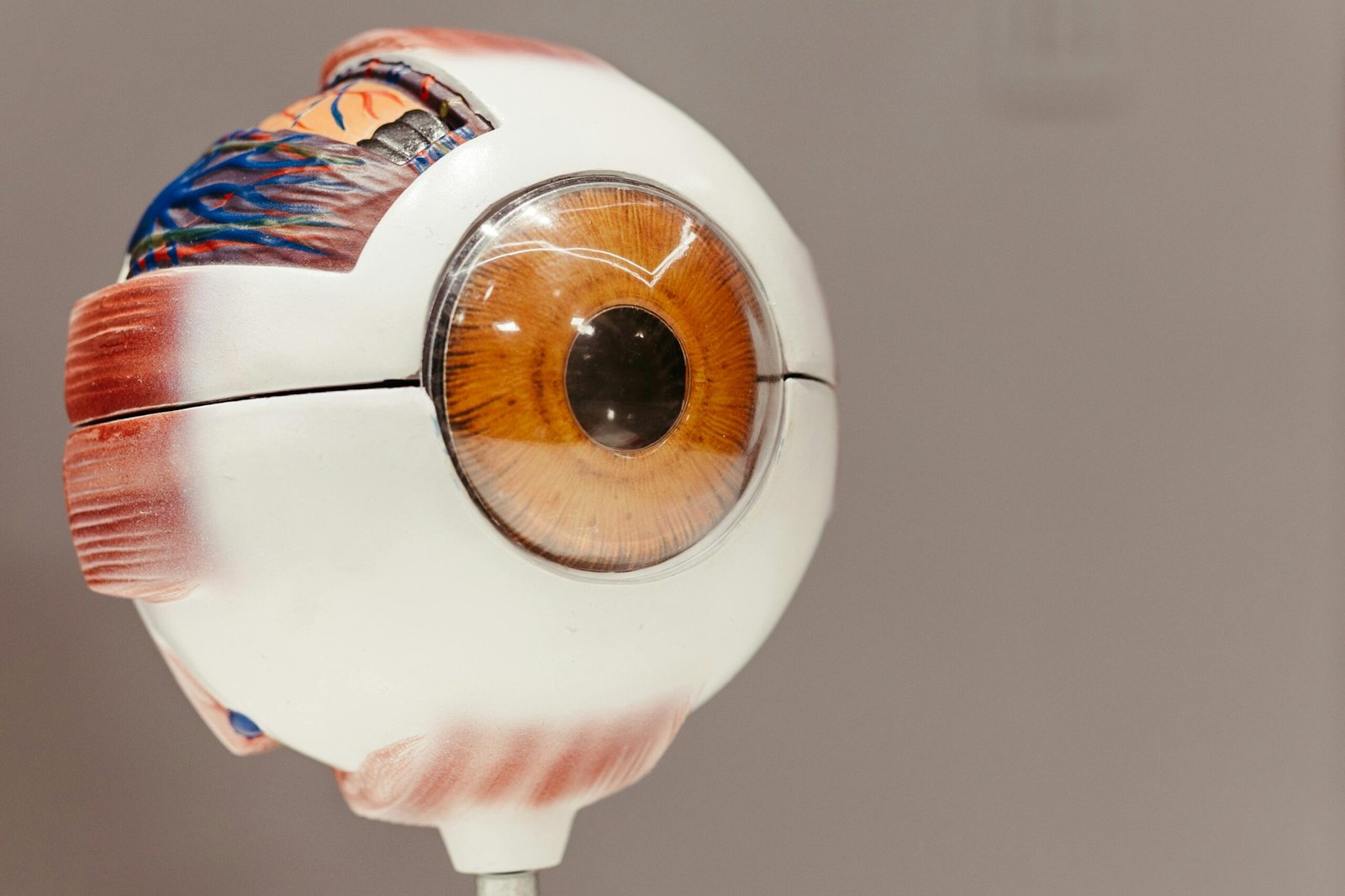
Diabetic retinopathy is a significant area of concern to people with diabetes since it has been a major cause of blindness to the working population in the world. This is a situation in which the excessive level of sugar in the blood destroys the small vessels present in the retina that is a light sensitive layer present in the back of the eye that is necessary to obtain vision. An essential role in healthy retina is the blood-retinal barrier (BRB) that serves as a gatekeeper between the blood and the retina regulating the entry and the exit of nutrients and wastes as well as fluids. By the disintegration of the inner part of this barrier, the inner blood-retinal barrier (iBRB), toxic substances may leak into the retina and trigger swelling with a possible loss of vision.
What is Diabetic Retinopathy?
Retinopathy occurs when there is progressive damage to the retina of the eyes of individuals with either type 1 or type 2 diabetes which usually do not show symptoms in advance. As the condition advances, a person can suffer blurred vision, floaters, compromise night vision or even blindness in case of no antidote. Routine eye examination is important and when it is done early, adequate treatment can be taken to slow down or prevent further severity. The disease isespecially worrying as it attacks the neurovascular unit of the retina which is a complicated web of blood vessels and nerve units which are vital in producing a proper vision.

The Diabetes Hypoglycemia Paradox
Blood sugar within the target range of control is one of the main pillars of complications in diabetes such as diabetic retinopathy. But the process of reaching a tight glycemic control may occasionally cause hypoglycemia one in which the level of blood sugar is too low. Low blood sugar is also improving retinopathy; this presents a difficult and complicated time to both patients and medical practitioners, though high blood sugar is certainly a legendary testament to retinal damages.
A new paper published in Science Translational Medicine on April 30, 2025, headed by scientists at the Wilmer Eye Institute at Johns Hopkins Medicine, gives new insights into this paradox. The article is a research study of diabetic mouse eyes, which explains the effects of hypoglycemia on damaging the retina and provides the possibilities of lessening this damage.
Key Findings from the Study
The researchers found out that hypoglycemia activates the deposition of two proteins, hypoxia-inducible factor-1, alpha (HIF-1, alpha and Hif-2, alpha in the retina system of diabetic mice. Vasoactive mediators are secreted as a result of these proteins, which under normal conditions are activated by the presence of low oxygen but in this case are stimulated by low glucose levels, and lead to the breakdown of the vessels walls in a situation also known as vasoactive response. So-called vesicular transcytosis permits the extravasation of fluids and proteins in the retina, breaking iBRB, and thus leading to vision-threatening pathological changes.
To validate such results, advanced technologies including gene expression levels of the retina during the low glucose conditions via RNA sequencing method were also incorporated by the team. They observed important induction of blood-vessel leakage-related gene and especially of those mediated by the transcription factors HIF-1alpha and HIF-2alpha. They also applied Evans blue dye as a method to measure vascular leakage, which indicated higher leakage in retinas of diabetic rodents with hypoglycemia than on those of the non diabetic rodents.
The investigation also manifested the use of diabetic and non-diabetic mice and only diabetic mice showed increase in HIF status under conditions of hypoglycemia resulting in the occurrence of iBRB disintegration with blood vessel seepage in the retina. This particular detail highlights the unusual sensitivity of diabetic retinas towards low blood sugar conditions.
| Key Experimental Methods | Description |
|---|---|
| RNA Sequencing | Analyzed gene expression changes in retinal explants under low glucose conditions, identifying HIF-regulated genes. |
| Evans Blue Dye Testing | Quantified retinal vascular leakage in diabetic mice, showing increased leakage during hypoglycemia. |
| HIF Inhibition | Tested the drug 32-134D to block HIF-1α and HIF-2α, preventing iBRB breakdown. |
Possibilities of the New Treatments
Among the most favorable observations that the research revealed is the efficiency of one experimental drug, 32-134D, that suppresses activities of HIF-1 and HIF-2. Once given to diabetic mice prior to induction of hypoglycemia, 32-134D was able to suppress the increase in HIF levels, and, accordingly, functioned to inhibit the release of vasoactive mediators, as well as to maintain the iBRB intact. This is an indication that HIF inhibitors may provide new therapeutic solution in diabetic retinopathy especially in cases where patients are at risk of hypoglycemic attacks with tightened glycemic control.
The results of the study have attracted attention in medical circles and clinic trials begin to assess the efficiency of 32-134D in humans with diabetic macular edema, a typical symptom of diabetic retinopathy, in which fluid leaks into the macula or the central visual field of the retina. In case of success, this medication would find a specific cure to stop or minimize vision impairments in diabetic patients.
Treating Sugar Level
The study shows how diabetes management is a fine line to balance. Although it is well known that high levels of sugar in the blood, aka hyperglycemia, possess a risk of progression towards diabetic retinopathy, this research demonstrates that a low level of sugar in the blood, aka hypoglycemia, may have severe consequences as well. The patients should collaborate with their caregivers to regulate the level of blood sugar and prevent excessive drops and spikes. The use of technologies, such as the continuous glucose monitoring systems could be effective as it gives the real-time data to achieve better control and minimize the risk of hypoglycemia.
Conclusion
The study will give a critical insight on the role that hypoglycemia plays in facilitation of diabetic retinopathy, through the activation of HIF-1 and HIF-2α which results in degrading blood-retinal barrier. Having discovered a molecular mechanism underlying this process, the study offers an interesting solution to how tight glycemic control occasionally exacerbates retinopathy. Besides, the effective use of the HIF inhibitor 32-134D in protection of retinal damage in diabetic mice opens the new horizons of possibilities in the treatment. The findings in relation to the clinical trials may enhance better methods of preserving sight of the millions of diabetes patients throughout the world.