Liver fibrosis is a silent killer whose onset can be due to sustained damage in the liver, which is usually as a result of hepatitis, alcoholism or fatty liver malady. A surplus of scar tissue accumulates with time resulting in cirrhosis, liver failure or even cancer. No existing drugs are approved by the FDA to reverse fibrosis and managing it mostly boils down to management of the underlying cause.
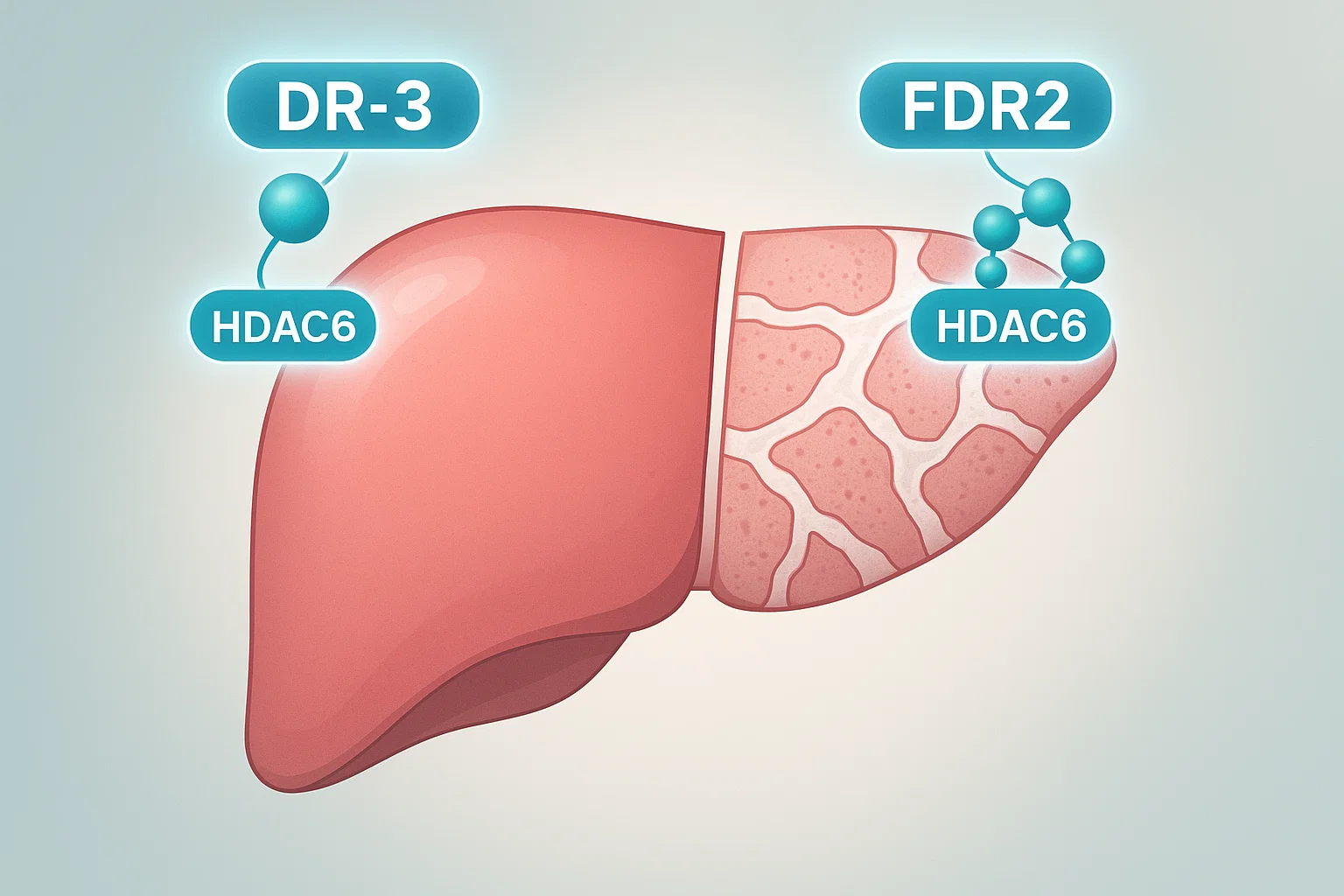
But there is a trailblazing study published at The FEBS Journal (2025). Two highly selective HDAC6-inhibitors dr-3 and FDR2 that bear an astonishing potential to slow down (and potentially reverse) liver fibrosis were developed by researchers.
What is Liver Fibrosis and Why is It So Dangerous.
Repeated injury of the liver by either viruses, toxins, or metabolic diseases causes a reaction known as scar formation that consists of scar tissue made by the liver. This is characterized by fibrosis which is initiated by the hepatic stellate cells (HSCs). Usually, these cells keep vitamin A and contribute to the functioning of the liver. However, on stimulation (when induces myofibroblasts) they begin to secrete too much collagen and other proteins making liver stiff.
Without being curbed, fibrosis develops into cirrhosis, whereby the degree of scarring in the liver outweighs its functionality. At this point, there is no treatment except liver transplant- it is expensive, risky and shortage of donors.
The HDAC6 in Liver Fibrosis
Histone deacetylases (HDACs) refer to gene expression regulating enzymes which work through changing proteins. Although certain HDACs maintain normal cell functioning, it is believed that HDAC6 has been associated with development of fibrosis. In this study, it was found that:
Increased HDAC6 present in fibrotic liver, with a high concentration above advanced fibrosis (F2-F3 fibrosis).
HDAC6 enhances the activation of HSC consequently resulting in increased production of collagen and scar tissue.
Reducing HDAC6 can decrease indicators of fibrosis in human liver tissue models.
That is why HDAC6 is a good target of anti-fibrotic medication.
DR-3 and FDR2: The Breakthrough
The study collective created 2 new substances DR-3 and FDR2 that choose HDAC6 but do not have an impact on other HDACs. That is why they are promising:
Selectivity and Effectiveness
The two inhibitors were found to be 100 times more selective towards HDAC6 as opposed to HDAC1.
They successfully augmented acetylation of α-tubulin, which is an important process in the decrease of fibrosis.
They reduced collagen, TIMP-1 and alpha-SMA which mark fibrosis in human liver cells (LX-2 LX).
Repressed TGF-beta 1 Signalling
Fibrosis is strongly driven by TGF- 1. In the study, it was observed that:
When TGF-ase was stimulated by TGF-1, DR-3 and FDR2 inhibited TGF-1-mediated SMAD3 activation, and thus, formation of scar tissues was evaded.
This was observed through human liver cells as well as rat HSCs indicating a potential wide scope.
Dampened Fibrosis in Human Livers Slices
Human precision-cut liver slices (hPCLS), a model highly resembling real liver tissue, provided the best pieces of evidence.
Both the inhibitors minimized the deposition of collagen as well as action of the myofibroblast.
Remarkably, FDR2 was very effective, even reducing background fibrosis in untreated samples.
Significantly, the medicines did not affect the liver cells as observed with LDH and albumin.
The Reason This is Important to Future Treatments
Available anti-fibrotic agents have the following two problems:
Imprecision-most of them act on more than one pathway and lead to side effects.
Material insufficient human data– majority of the studies use animal models that may not be applicable to human beings.
In this case, this study goes over both of these hurdles:
DR-3 and FDR2 are highly selective with off-target effect reduced.
hPCLS models have the benefit of offering human-relevant data boosting the level of confidence regarding clinical possibilities.
To the clinic to scale: Next Steps
Though the findings are thrilling, more studies should be carried out:
The metabolic-associated steatohepatitis (MASH) models when fatty liver disease is a major contributor to fibrosis however is only tested in.
Long term safety studies – to make sure that there is no latent toxicity.
Clinical trials– to verify effectiveness in people.
Conclusion: New Hope in the Treatment of Liver Disease?
The fibrosis of the liver has become a silent epidemic as little can be done to treat it. The finding of DR-3 and FDR2s has the potential of altering that. The use of acquired HDAC6-directed inhibitors provides a specific, effective and safe means of fighting fibrosis.
provided that studies in the future prove their effectiveness, soon we might have the first real anti-fibrotic drug; that is not only slows the disease but is possible to even partially correct liver damage.
It could actually save the lives of millions of people who have chronic liver disease.
Reference:
Borrello, M. T., et al. (2025). Pharmacological manipulation of liver fibrosis progression using novel HDAC6 inhibitors. FEBS Journal.
https://febs.onlinelibrary.wiley.com/doi/pdf/10.1111/febs.70062