Next-generation pacemakers have revolutionized cardiac care, combining tiny implantable devices with pioneering biological approaches. The 2018 Cedars-Sinai study, ‘Next-generation pacemakers: from small devices to biological pacemakers,’ showcases how modern leadless designs and living-cell therapies may soon replace bulky, traditional devices.
Why Pacemakers Matter for Heart Health
The Sino atrial node (SAN) works as an inherent cardiac electrical conductor which holds its position at the tip of the right atrium where it controls the heartbeat as a tiny cluster of cells behaves like a drummer. The electrical network silently operates heart functions at the same time it regulates blood circulation throughout a lifespan that equals 3 billion heartbeats. But sometimes, things go wonky. Diagnosis in the Sino atrial node along with other heart electrical structures leads to unusual beat patterns and fainting events.
The heart system finds backup from pacemakers that contribute regular heart rhythms during main system failures.
This paper emphasizes the vital importance of this technology because unborn babies with congenital heart block have an 80% mortality rate when they lack proper heart rate control. Survival chances for infants with stopped hearts depend completely on immediate medical treatment because their death risk remains dangerously high. The lifesaving technology of pacemakers has existed since 1950s yet they continue to have various functional limitations. The article examines present-day attempts to develop better cardiac devices and live heart cell technology alternatives for pacemakers.
Old-School Pacemakers: Clunky but Clutch
Pacemakers entered the medical market during the 1950s with an initial struggle period. The early pacemakers appeared as large devices that connected patients to substantial equipment through chest-wired units while maintaining a bothersome appearance. During 1958 Swedish inventors shifted medical history with their initial deployment of an internal pacemaker. The device managed to survive for just three hours which marked the beginning of this system.
The implantable pacemakers of the 1960s used mercury batteries (yikes). Lithium batteries became commercially available because they offered battery life lasting approximately ten years and continue being used in the present day.
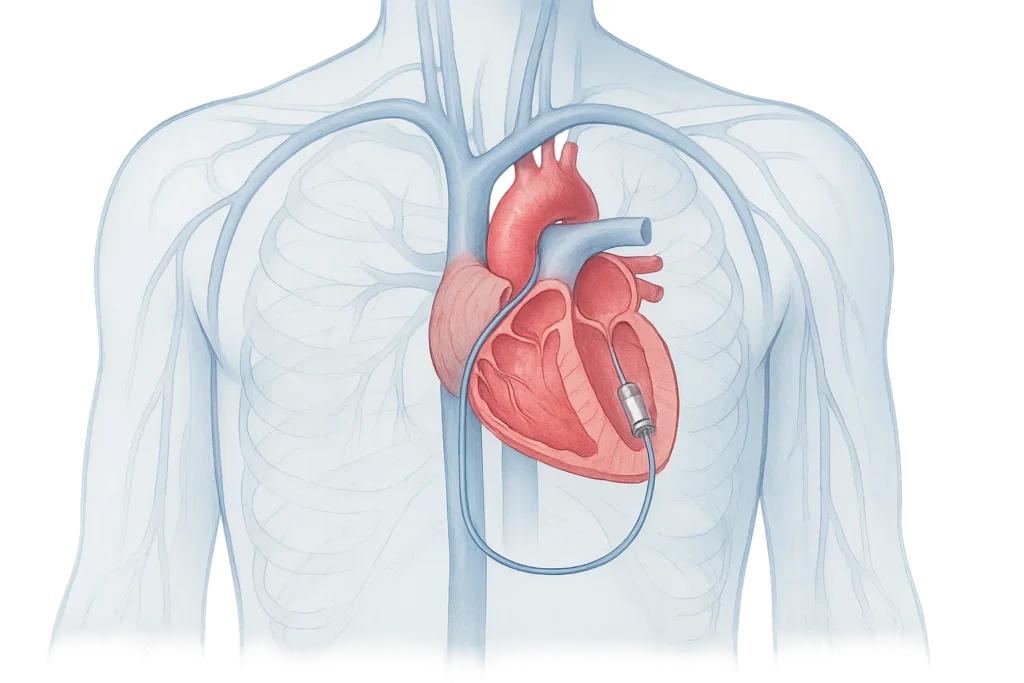
Pacemakers in the present era function through small implants under the skin and deliver power to the heart through thin wire leads. The device recognizes your body’s natural heart rhythms before offering assistance only in specific needed situations making it truly impressive. The medical procedure of pacemaker implantation happens to more than 200,000 Americans annually.
Still, problems remain. The pacemaker leads show two problems during their production stage they might break apart or produce microbial infections and they can damage heart valves. The replacement of exhausted batteries leads to additional operations. Your heart requires help from a pacemaker to build rate naturally during exercise or stress.
The New Kids: Leadless and Fancy
The paper discusses emerging innovative technologies. First up: ledless pacemakers. Speak to a professional about receiving these diminutive devices which get inserted straight into your right ventricle through your leg’s vein without surgical incisions. The treatment procedure decreases infection likelihood while providing better comfort for patient care.
The downside? A single-chamber restriction limits the use of leadless pacemakers as an appropriate treatment for all patients. The insertion of these devices demands use of a substantial-diameter tube which does not seem optimal.
Scientists use His-bundle pacing technology to direct a pacemaker toward heart fibers which produces more natural heartbeat coordination for reduced heart strain. The combination of connecting both heart ventricles with biventricular pacing improves heart failure patients but its success rate is not always ideal.
Experts explore two experimental pacemaker designs that employ sunlight through the skin and heart motor energy to recharge themselves. How wild is that?
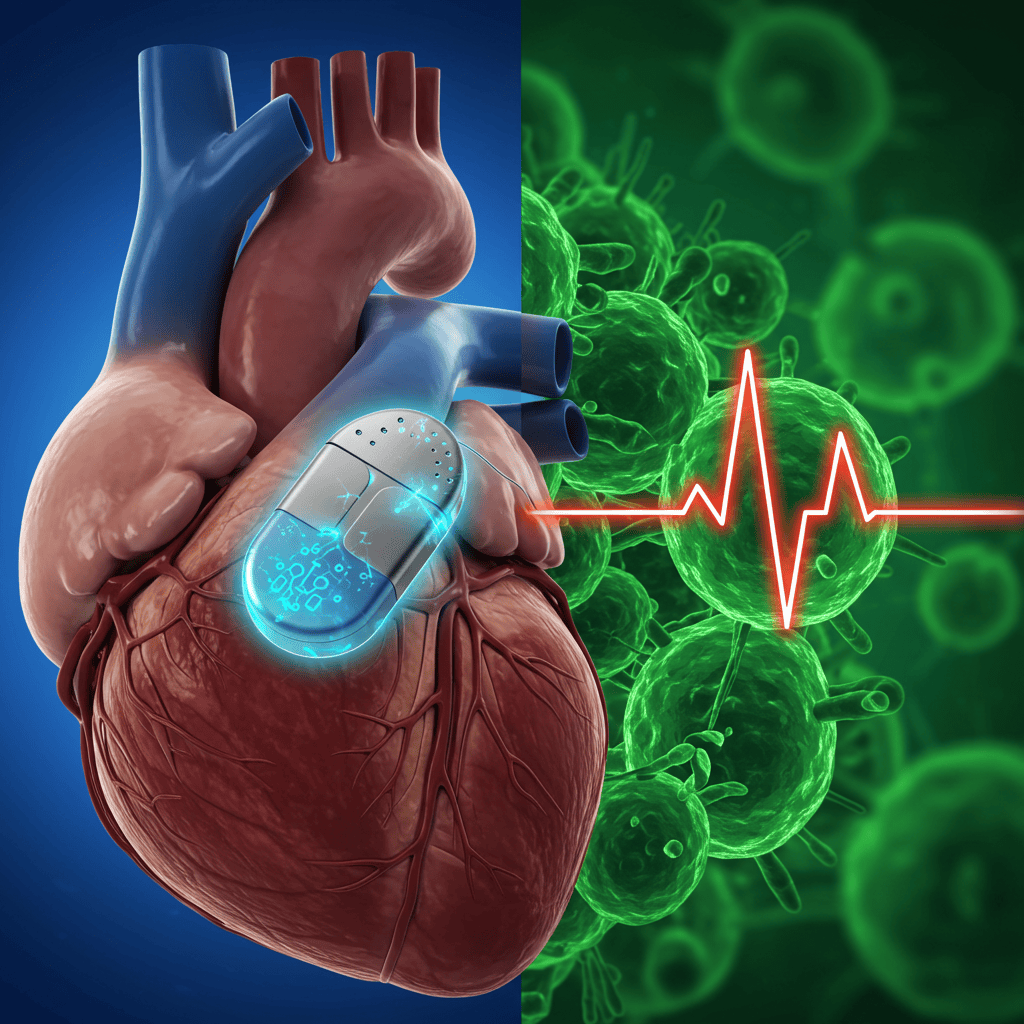
Biological Pacemakers: Your Heart as the Fixer
Here’s where it gets mind-blowing. Would it be possible to eliminate both the need for metal devices along with wires? Heart cells in your own body could eventually serve as an automatic pacemaker for your heart.
Biological pacemakers bring a transformative way to address this medical problem. Scientific researchers have identified various practical methods for this research.
Researchers adopt gene therapy approaches to produce new pacemaker cells through genetic modification of heart cells using HCN2 (part of the “funny current”) genes. Successful research results have been achieved by scientists through their development of pacemaker regions in dog hearts. Scientists use a technique that stops I_K1 potassium currents from functioning to obtain automatic heart cell beating. The method exhibits difficulties because it may make heart cell activity rhythmic but disorganized.
Scientists develop heart cells from either embryonic stem cells or by implementing the stem cell characteristics in skin cells known as iPSCs. Researchers have obtained different outcomes when they inserted these elements into animal heart tissues. Patients have to take medication following receiving biological pacemakers because the native environment of the body remains challenging to support these devices. The paper’s got all the juicy details (check it out at DOI: 10.1038/nrcardio.2017.165).
References & Further Reading:
Original study: DOI: 10.1038/nrcardio.2017.165.