Skin cancer is considered as one of the most prevalent cancers all over the world with millions of new cases being reported annually. The survival rates are much better when cell lesion is diagnosed early, yet professionals in a specialized field, expensive imaging devices, and manual analysis of developed images are often necessary in skin lesion diagnosis. Most recently, a new study that also represents an AI-driven deep learning technology has been developed which can identify skin lesions in a speedy, accurate, and even high-volume way, which could revolutionise dermatology and bring early diagnosis to even more people.
The Problem with Skin Lesion Diagnosis
Dermoscopic image and visual inspection are important instruments to dermatologists to identify suspicious moles or lesions. As much as it works, this process has its limits:
Subjectivity: It is possible to diagnose different specialists.
Time Constraints: The large number of patients leads to analysis that may take time.
Access Barriers: Underserved/Rural communities might not have trained dermatologists.
That is because midway in this timely and regular diagnosis lies failure of some cancers to be diagnosed in good time, which may limit treatment possibilities and survival.
The AI Breakthrough
The study group created a profound convolutional neural network (CNN) that was trained using thousands of dermoscopic photos using freely available databases like HAM10000, PH2, and ISIC. The model was trained to do classification of several types of skin lesions, such as:
Melanoma is the type of skin cancer that is deadly.
Basal cell carcinoma– slow-growing and common although they require elimination.
Benign moles– non cancerous but may look like or take after cancerous lesions.
It trains the AI system on lots of labeled images as the system learns to identify the subtle differences in shape, color, and texture that is often well below human perception.
How It Works
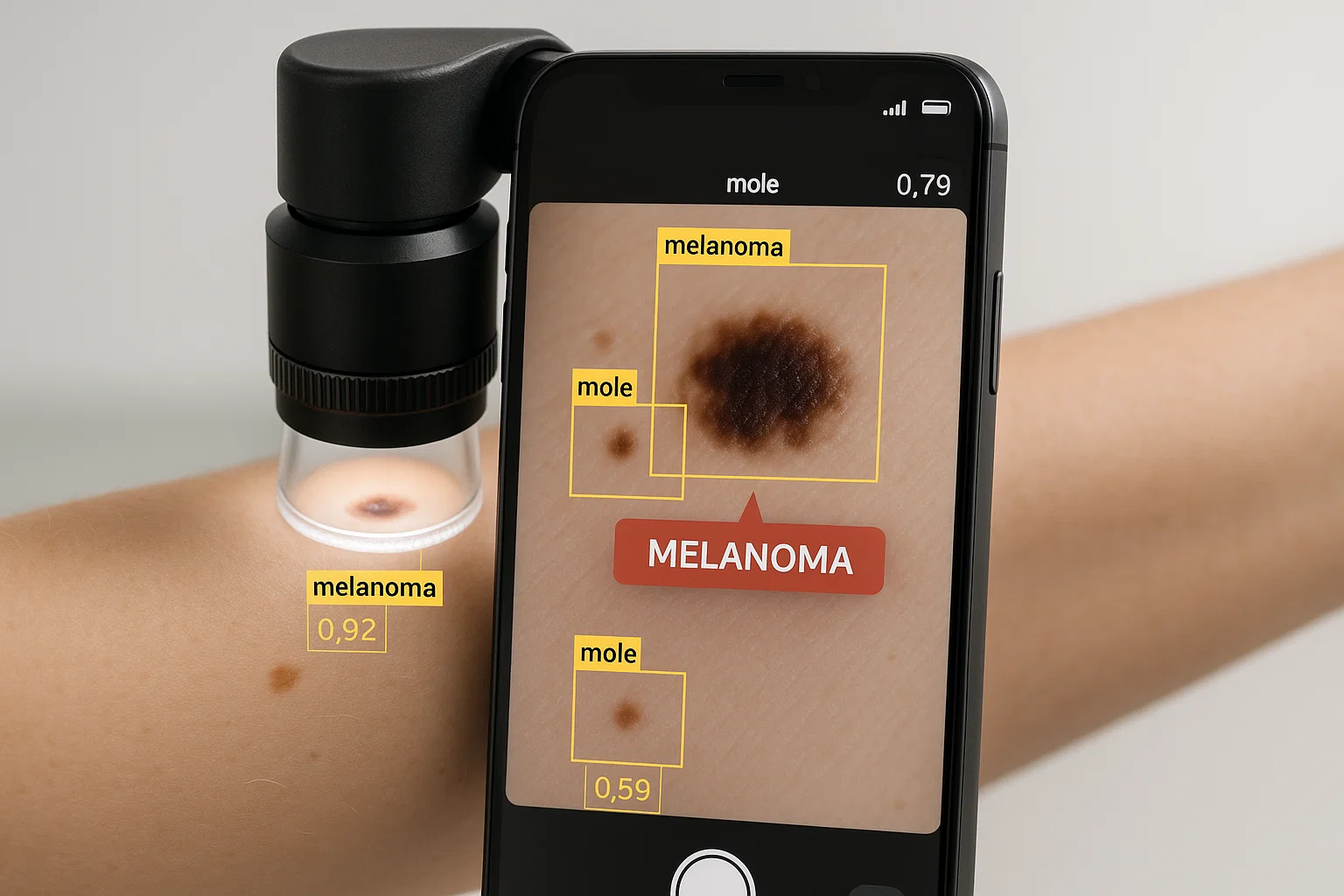
Image Acquisition: Image acquisition is performed by use of a special camera or even a smartphone and lens attachment.
Preprocessing: The images are cleaned, resized, and normalized so that the same analysis is carried out.
Feature Extraction: CNN than the camera automatically detects asymmetrical, border irregularity, color variations, which are warning signs of melanoma.
Classification: The AI applies classification to the lesion and assigns the lesion to several categories of diagnosis at a probability percentage.
Performance Results
The AI was able to attain an accuracy of more than 90 percent in test datasets-equaling or beating the diagnostic accuracy of trained dermatologists in controlled trials. It also proved:
High Sensitivity: Senses the cancerous lesions with little false negatives.
High Specificity: The test does not generate too much false positive that may result in unnecessary biopsies.
Speedy Processing: Provides an outcome in seconds, as opposed to minutes or hours with a manual review.
Advantages Over Traditional Diagnosis
Speed: Rapid analysis assists in accelerated clinical decisions.
Scalability: It can be scaled to use in clinics, mobile health units or telemedicine platforms.
Cost-Effectiveness: Costa-effective due to lesser unnecessary specialist referrals.
Consistency: Eliminates variability of diagnostic amongst physicians.
Possible Real-World Use
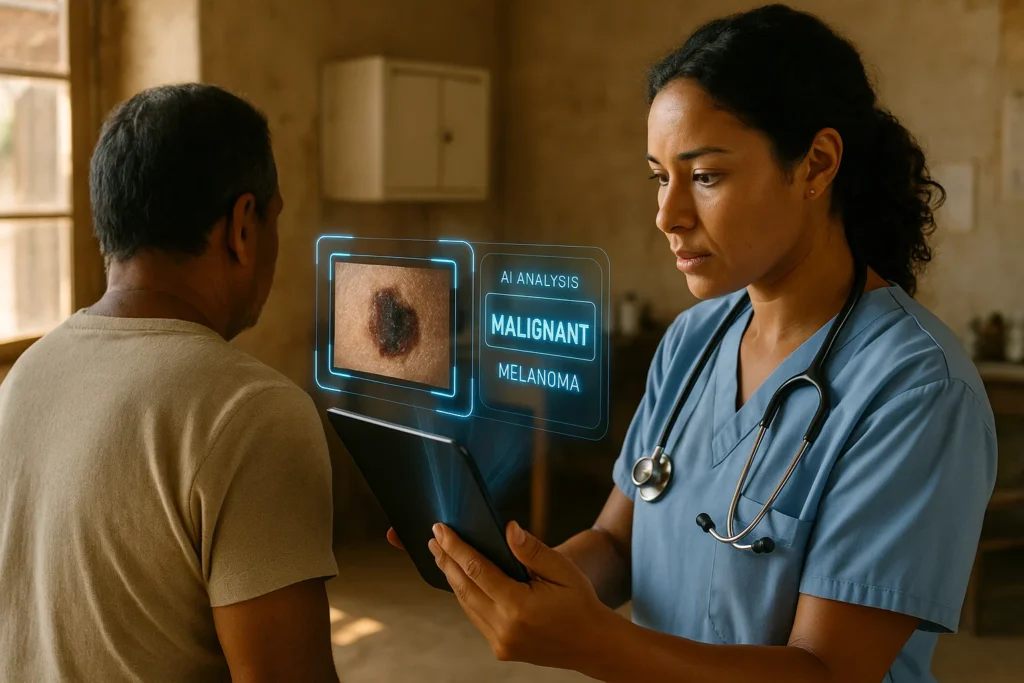
Teledermatology: Patients may transmit images remotely so that they can be reviewed immediately with the help of AI.
Dermatology in Rural Healthcare: Reliable screening can even be provided by clinics without dermatologists.
Preventive Care: Increases the utilization of more often skin examinations among risk groups.
Research Support: Assists in evaluating large quantities of images in a more effective manner.
Constraints and Future Studies
Although the AI model demonstrates an impressive performance, it still has to overcome obstacles on its way to becoming widely adopted:
Bias in dataset: Any model trained on a limited skin type can be poorly adapted to minority groups.
Integration Issues: Would have to integrate with current workflows in healthcare.
Regulatory Approval: Has to undergo clinical trials and must acquire certifications before being used in clinic.
The aim of the researchers is to grow training sets, enhance their robustness and incorporate the tool with several mobile health apps to be used by the population.
Effect on Public Health
When extensively implemented, this AI technology has the potential to drastically cut the time between the incident and the diagnosis, and also, it can increase the early cancer detection rates and save lives. In the case of countries where few dermatology professionals exist, AI-enabled technology may become a lifeline of early prevention- detecting melanoma and other potentially life-threatening skin diseases before it is too late.
Conclusion
The introduction of AI and deep learning to dermatology is a huge leap towards skin cancer detection. Its new system is fast, precise and of a scalable nature thus assisting in closing the gaps in access to quality healthcare. As the human expertise is still essential, AI can be its strong companion that gives power to doctors, increases access to patients, and eventually saves lives.