Chronic wounds and severe burns remain a major challenge in modern medicine. Despite decades of advances, current treatments such as skin grafts, cultured epidermal autografts, and synthetic matrices often fail to regenerate functional dermal tissue. Instead, patients are left with scars, limited elasticity, and compromised healing. According to the World Health Organization, more than 11 million people require hospital treatment for burns annually, with 180,000 deaths worldwide.
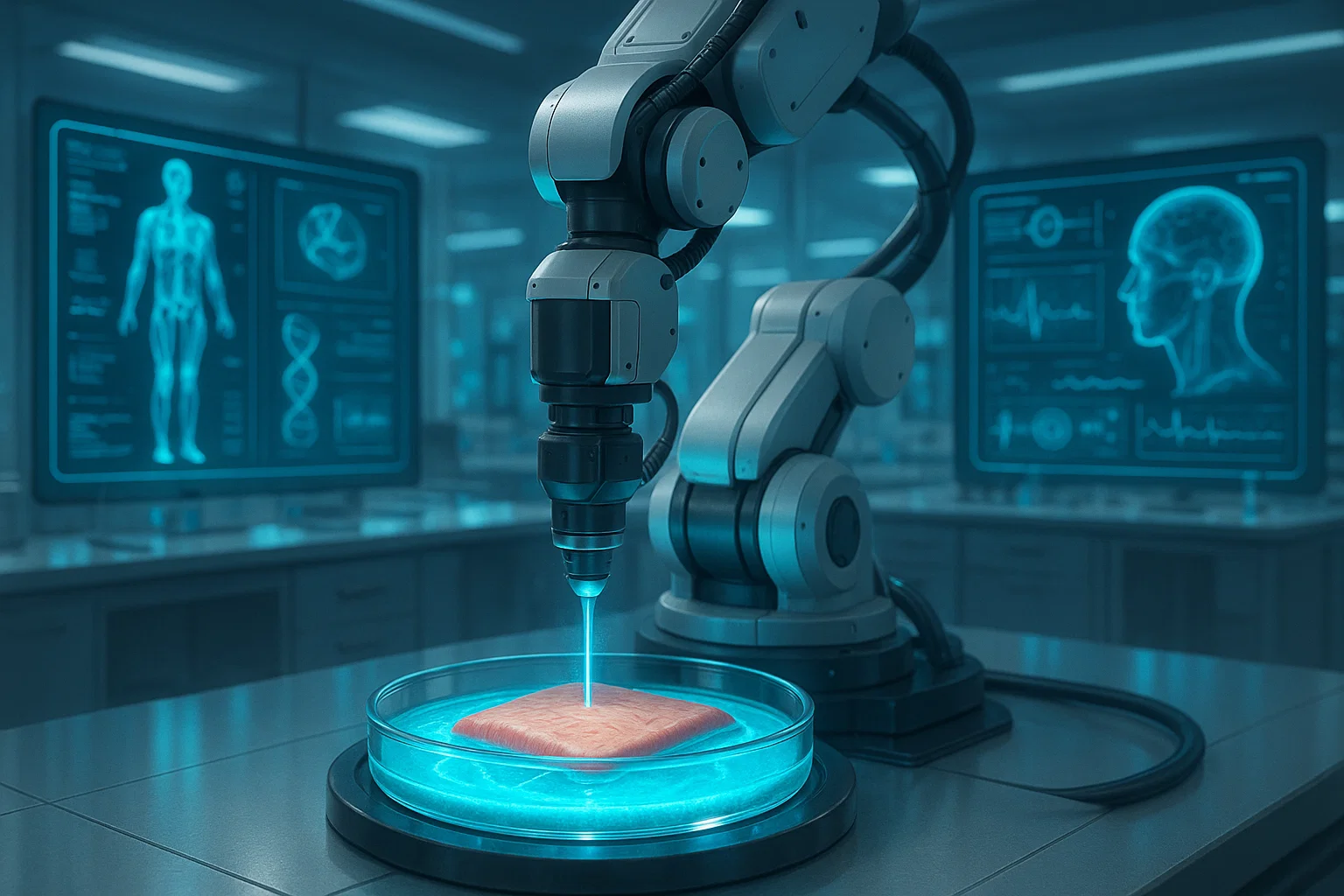
A new study published in Advanced Healthcare Materials introduces an innovative approach: biphasic granular bioinks (µInk) a 3D bioprintable material designed to generate ultra-high cell density constructs that mimic natural skin and promote scar-free healing.
The Reason Current Treatments Are Inadequate
The conventional forms of wound healing; the split-thickness skin grafts and the engineered dermal substitutes merely reconstruct part of the skin structure. They are so liable to:
This is due to low cell density, which restricts integration of tissue.
Slow extracellular matrix (ECM) production → delaying natural healing.
High scarring risk → reducing functionality and aesthetics.
The above-presented limitations introduce the necessity in developing innovative methods capable of simulating diverse extracellular structure and dynamic functions of dermal fibroblasts in skin regeneration
The Innovation Biphasic Granular Bioinks (uInk)
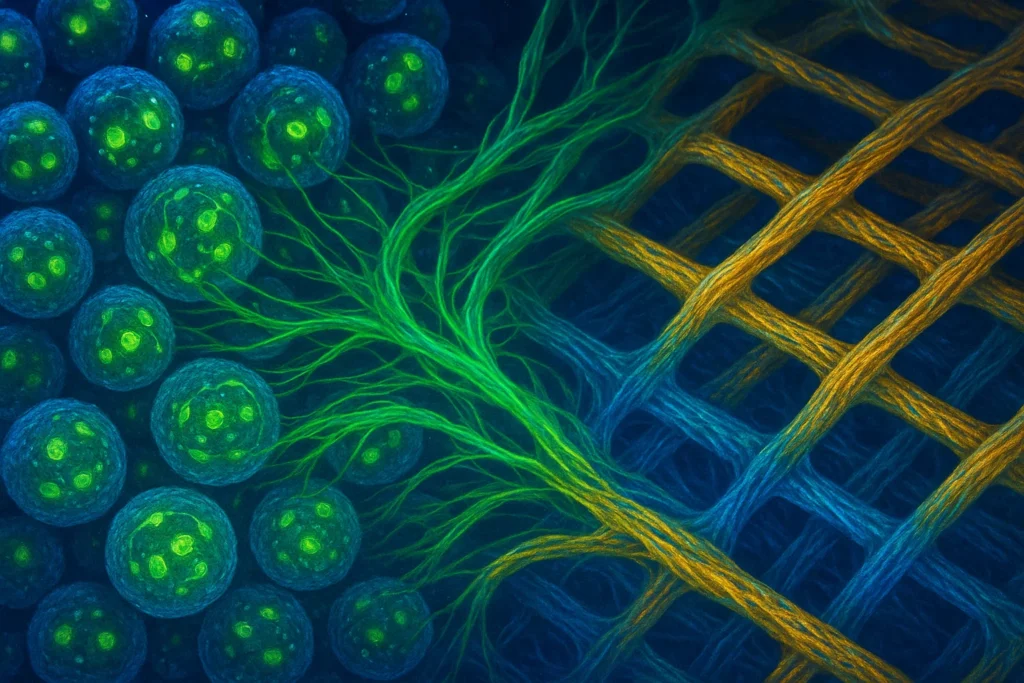
The research group created a bioprintable biphasic granular hydrogel bioink that consisted of cell-laden porous gelatin microcarriers (PGMs). They are mixed with a hydrogel based on hyaluronic acid by the means of copper-free click chemistry to form a shear-thinning, structurally stable, and biocompatible medium
Key Features of µInk:
Ultra-high cell density: fibroblasts are grown on PGMs in the bioreactor prior to printing, leading to cell-rich scaffold.
Bio printable 3D: µInk provides shape fidelity to produce multilayered dermal structures.
Biocompatibility: cells are not killed, reproduce and do not change phenotype after transplantation.
ECM production: transplanted fibroblasts secrete collagen, elastin, and laminin, essential for natural dermal regeneration.
Scar-free healing potential: promotes neovascularization (new blood vessel formation) and tissue remodeling.
The Way It Works
Cell Expansion: Human dermal fibroblasts (HDFs) are allowed to expand in the bio-regulated bioreactor environment on PGMs.
Bioink Formation: The PGMs loaded with cells are cross-linked using a hyaluronic acid/PEG hydrogel using click chemistry.
3D Bioprinting Across: 3D bioprinting in the 3μink enables the airway-JW scaffolds to be formed and stabilized by the extrusion bioprinting method into stable dermal scaffolds.
Transplantation: After the cells are implanted they multiply, remodel the hydrogel, and deposit natural ECM.
Healing Result: The constructs blend well to the host tissue without causing fibrosis and scarring
Experimental Highlights
Post printing Viability: Cell viability was maintained above 75 %.
In Vivo Success: Embedded constructs in animals model embedded 28 days of tissue integrations and vascular development.
Dermis type ECM: Skin architecture was recreated with the production of collagen I, III, IV, laminin and elastin.
Lower Scarring Risk: µInk promoted the production of regenerative pathways as opposed to fibrotic pathways as opposed to when fibroblast spheroids are formed, causing inflammation and fibrosis, in many cases.
Clinical Implications
The breakthrough promises:
Burn victims Burn victims: Allow functional regeneration of skin without severe scar actions.
Chronic wound patients, in particular diabetics and older populations that experience slow healing.
Reconstructive surgery: providing natural tissues as opposed to the synthetic implantation.
Personalized medicine: Personalized/tailoring of bioprinted constructs to increase compatibility using patient-derived cells.
If successfully translated to clinical practice, µInk could dramatically reduce healthcare costs (estimated at $96.8 billion annually in the U.S. for wound care), while improving quality of life for millions worldwide.
Conclusion
Biphasic granular bioinks open a new window to regenerative medicine. With a combination of 3D bioprinting, ultra high cell density, and biocompatible materials, an avenue of scarless wound healing and functional dermal regeneration has been developed by the researchers.
Other than solving medical problem long overdue, this innovation is a step towards realizing the vision of lab grown, which we can use in a personalized approach to medical care.
References & Resources
Shamasha, R., Ramanathan, S. K., Oskarsdotter, K., et al. (2025). Biphasic Granular Bioinks for Biofabrication of High Cell Density Constructs for Dermal Regeneration. Advanced Healthcare Materials. DOI: 10.1002/adhm.202501430
World Health Organization Burn Fact Sheet
National Institutes of Health, Extracellular Matrix in Wound Healing