A blood cancer known as leukemia has always been a major problem among medical researchers and also the patients. Conventional therapies such as chemotherapy are highly associated with mild and disabling effects as well as different recovery percentages. Nevertheless, a landmark work in the journal Nature Biomedical Engineering offers a paradigm changing invention: a bioengineered immune-competent preclinical trial on chip. Its new technology replaces the human bone marrow niche and provides an innovational method of sorting leukemia CAR T cell treatments with an accuracy that has never been seen before. This blog looks at how this innovative process may be the sea change in cancer treatment, and the resultant outcome of this practice with the general reader in mind.
What is CAR T Cell Therapy?
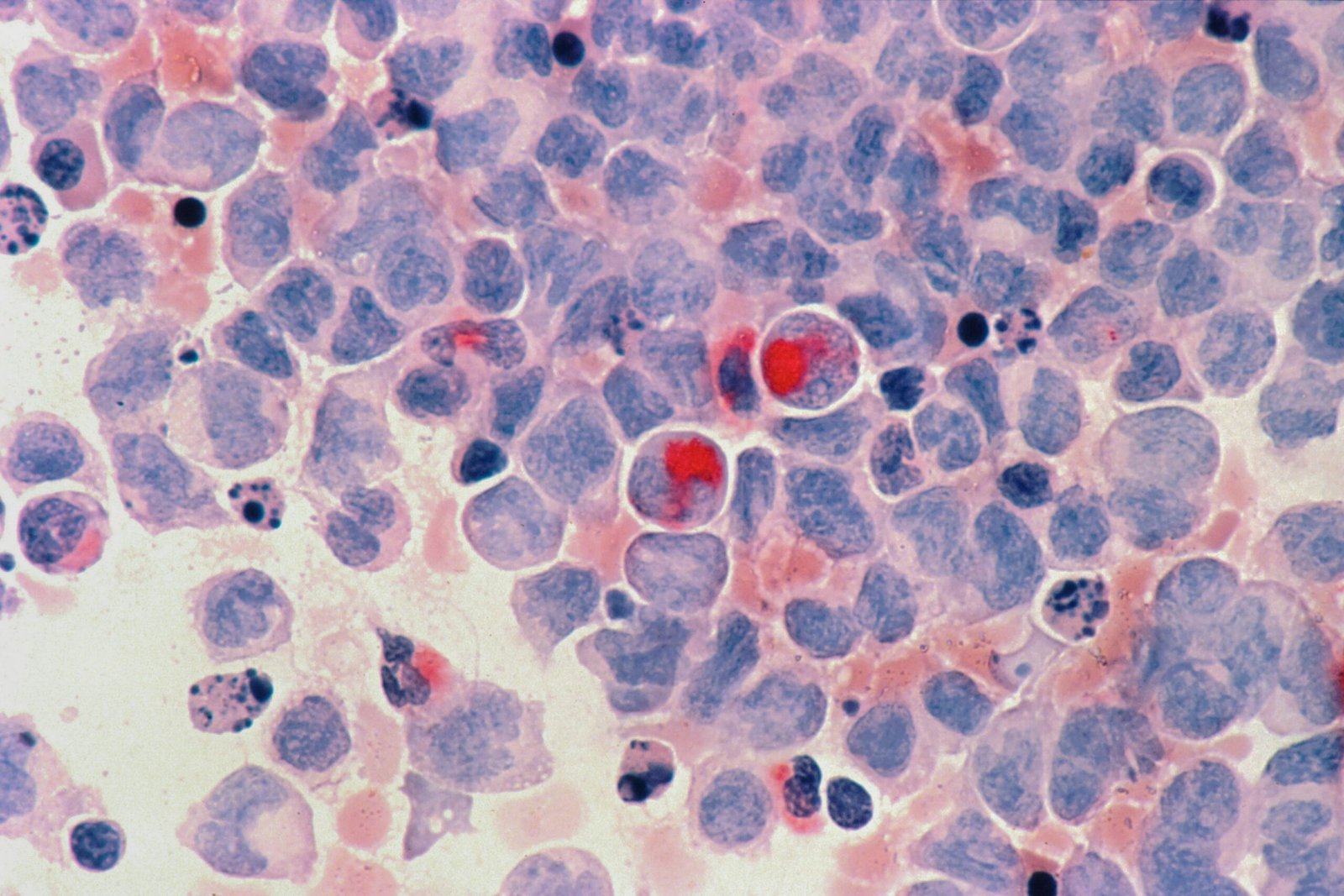
One such therapy is Chimeric Antigen Receptor (CAR) T cell Therapy which has so far demonstrated great success in the treatment of some types of leukemia more so B-cell acute lymphoblastic leukemia (ALL). During this treatment, T cells (a kind of immune cell) in a patient are taken apart and transformed in a lab to target and demolish cancer cells that represent definite markers, e.g., CD19. Although CAR T cells therapy has resulted in remission in several patients, its efficacy has not remained the same since it is influenced by diseases resistance, relapse, or lack of variation in the T cell activity. This inconsistency highlights the necessity of improved preclinical test methods to be able to forecast the success of therapy.
The Problem with Preclinical Testing
There are deficiencies in traditional preclinical models, as exemplified by animal testing or in vitro assay. In animal models, the pathway of human immunity is often quite different to models, and its preparation is time-consuming, with no ability to accommodate real time monitoring. Although less complex, in vitro platforms fail to demonstrate the intricate microenvironment which occur in the bone marrow, the place where leukemia occurs. These deficiencies decrease the predictive value of the preclinical tests, and it is more problematic to know which of the CAR T cell products will be beneficial to individual patients.
Enter the Trial-on-Chip Technology
The trial on chip technology the Nature Biomedical Engineering journal team wrote about will help solve the issues because it produces an ex vivo model of the human bone marrow niche. Heterogeneity of this microfluidic chip is seeded with human bone marrow cells which consist of hematopoietic, vascular and endosteal cells to mimic the in vivo-like situation in which leukemia proliferates. The design of the chip enables the observation of the behavior, including extravasation (leaving the blood vessels) and killing tumor cells, of CAR T cells in real time by the researchers.
The main characteristics of the trial on chip are:
Immunocompetence: The chip contains the human immune cells, and thus, it is more reflective of the immune system of a patient.
High Throughput Screening: The researchers can compare the effect of a series of CAR T cell products to leukemia cells by testing them together.
Individualization: With patient derived cells the chip can simulate individual patient responses leading to the proposal of individualized medicine.
Key Findings from the Study
The research, conducted by a team of researches (Chao Ma, et al.), shows that this chip can simulate the major therapeutic response scenario such as remission, resistance, and relapse. Specifically, the chip precisely modeled clinical results in which CAR T cells highly attacked CD19 positive leukemia cells but not CD19 negative, resulting in the relapse due to the expansion of resistant clones that had existed before. Such is the same in the real-world cases, making the possibility of the chip as a predictor.
Another way in which the researchers used a comparison is between the various CAR T cell products, including D3 CAR and DP CAR and analyzed the performance of these products functionally, in terms of migration and persistence. They found markers (e.g., CD69) and T cell receptor sequences predicted therapy success or treatment failure by analyzing such techniques as flow cytometry and single-cell RNA sequencing. Such knowledge should inform the manufacture of better CAR T cells medications.
Why This Matters for Patients
As is the case with leukemia survivors, the trial on chip promises more practical and even personalized therapy. Screening CAR T cell products prior to administration can help the doctors to pick the therapy that would have the highest probability of inducing remission, yet with less chance of relapse. Such an individualized model would save trial and error measures, thus exposed patients would not be subjected to ineffective treatments and its side effects.
In addition, the capabilities that its chip has to simulate the resistance and relapse situations can make the process of finding new methods of overcoming these issues much faster. As a case in point, combination treatments or even second-generation CAR T cells (which deliver multiple antigens) might be experimented upon to fix the problem of antigen evasion.

Future of cancer treatment
The trial-on-chip technology is a breakthrough that introduces precision oncology. It has a high throughput immunocompetent design that makes it a generalizable tool not just in leukemia but potentially in other cancers that have complex microenvironments. As the technology develops, it may be combined with other technical achievements, including AI-based analysis of data, to make it even better at predicting the accuracy.
Nevertheless, it has set problems. The issues of cost, standardization, and regulation will have to be mitigated to scale the technology to a broader use by the clinical community. Also, the chip has strong resemblance to the bone marrow niche, but it might fail to represent all the human body components in their systemic responses towards treatment.
Conclusion
The trial-on-chip technology that is bioengineered is a game changer in this battle with leukemia. It acts as the interface between the preclinical research and successful clinical outcomes by offering a more patient-specific and realistic platform where CAR T cell therapies can be tested. To the patients, it may imply that they would receive prompt treatment and have a higher possibility of long term remission. This tool, which is still being perfected by the researchers, will have the capacity of reshaping the way we grow and administer cancer treatment options and achieve a better future in which personalized care will be the new norm.
Reference and Resource:
Ma, C., et al. (2025). Bioengineered immunocompetent preclinical trial-on-chip tool enables screening of CAR T cell therapy for leukemia. Nature Biomedical Engineering.
https://doi.org/10.1038/s41551-025-01428-2
National Cancer Institute: CAR T-Cell Therapy