Sudden cardiac death (SCD) terrifies both the patients and medical practitioners. This fear is especially critical among those who have hypertrophic cardiomyopathy (HCM) (the most common inherited heart disease, with a prevalence rate of about 1 per 500) the condition prevalws among the young in particular. The existing means of determining which individuals face the greatest risk of lethal arrhythmias (SCDA) are frustratingly inaccurate and have been producing both missed chances to prevent death in people currently destined to die, as well as unnecessarily invasive procedures on people that could never have suffered the fatal arrhythmia. With an innovative new multimodal AI tool called MAARS the landscape is about to change drastically.
What is Hypertrophic Cardiomyopathy (HCM)?
Consider that the heart muscle became thickened and especially the wall between its major pumping chambers abnormally thickened. It is HCM. Some individuals show symptoms such as shortness of breath, chest pains or faint, but others do not experience warning signs. The increased thickening might also interfere with the electrical system in the heart producing chaotic and fatal heart rhythms (ventricular arrhythmias) which is the major cause of sudden death in the youth, including hoopers.
Prediction Problem
The existing clinical risk-assessment recommendation to manage the SCDA risk among HCM patients (such as the ACC/AHA or the ESC guidelines, or HCM Risk-SCD calculator) is based on a limited number of variables, such as severe heart chamber enlargement, syncope of undetermined cause, family history of SCD, or abnormal cardiac rhythms on a monitor. However they are not always good and their performance may vary such that they may miss many of those at risk and declare many not at risk to be at risk (AUROC was ~0.51-0.62 in this study). This uncertainty results in great anxiety and prevention of implantation and excess of implantable cardioverter defibrillators (ICDs) which have costs, such as infection and improper shock.
Filling the gap: The MAARS: Multimodal AI to the Rescue
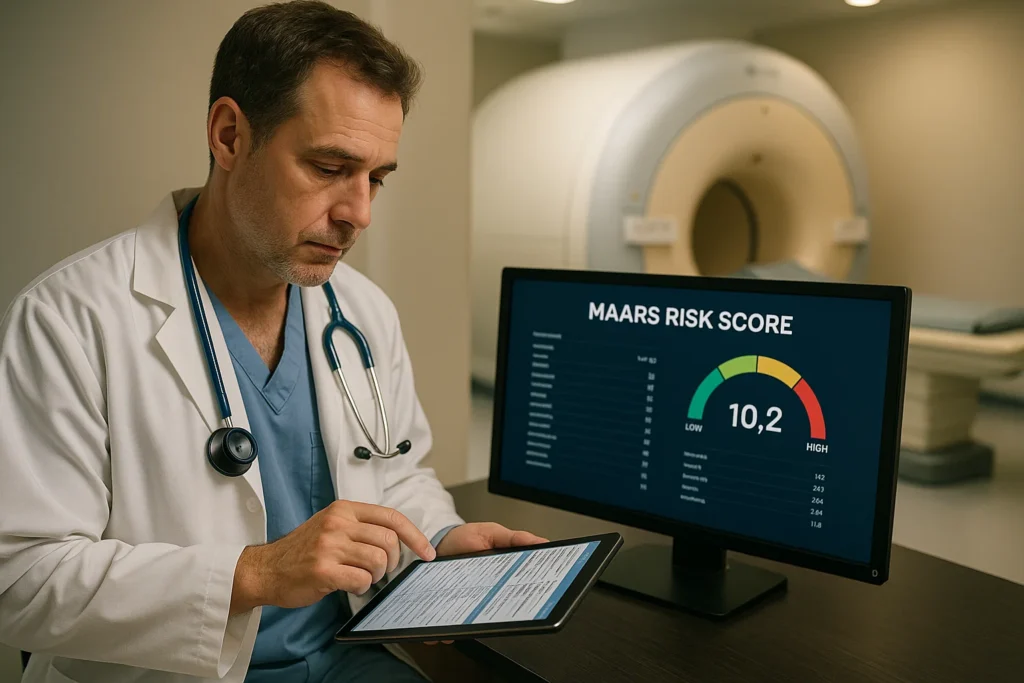
The MAARS (Multimodal Artificial Intelligence for ventricular Arrhythmia Risk Stratification), developed by Johns Hopkins University researchers and other institutions associates and reported in the journal Nature Cardiovascular Research is a paradigm shift. MAARS does not only count on a few of manually chosen features, but also uses the power of deep learning and incorporation of multimodal data to explore the whole picture of a patient:
Electronic Health Records (EHR): Demographics, past history, symptoms, family background, stress tests.
Cardiac Imaging Reports (CIR): Quantitative variables extracted Cardiac Imaging Reports (e.g., Echocardiogram (Ultrasound) and cardiac MRI reports: wall thickness, chamber sizes, valve function and outflow gradients).
As an important point, MAARS examines the unprocessed signal intensities of Late Gadolinium Enhancement Cardiac Magnetic Resonance (LGE-CMR) images directly. Those scans allow viewing of the scar tissue (fibrosis) inside the heart muscle which is a primary substrate of hazardous arrhythmias. Based on a hand-crafted 3D Vision Transformer (3D-ViT), MAARS can acquire the fine details nothing a human expert or simple model could see in the 3D scar distribution, and remove the variability of subjective interpretation.
How MAARS Works: Viewing the Big Picture
MAARS is not a black box to which data is hurled. It possesses an elaborate architecture:
Three Unimodal Branches: discrete neural networks (one is a 3D-ViT learning the patterns of the images, feedforward neural networks learning the patterns of the EHR and CIR data) initially learn deep patterns in each data type.
Multimodal Fusion Bottleneck Transformer (MBT): It is the integrator king. It absorbs the encoded information by each and every branch and learns about the interactions and combinations among the information in the various modalities toward prediction of SCDA risk, coming up with a complete representation of the patient.
Empathic Conclusions: Beating the Status Quo
MAARS had been stringently tried:
UnDeveloped (Internal Validation): 553 patients of Johns Hopkins achieved an AUROC of 0.89 (95% CI: 0.79-0.94). This implies that it properly placed a randomly selected high-risk patient above a low-risk patient, 89 percent of the time. It performed tremendously better than existing clinical guidelines with 27-35 percent difference in AUROC.
External Validation (286 patients in Atrium Health, NC): Most importantly, MAARS continued to demonstrate its efficacy (AUROC 0.81, 95% CI: 0.69-0.93), showing its transferability to represent a dissimilar patient population and healthcare system, and well above the guidelines by 22-30%.
Fairness: Instead of biased results, where many AI models were predominately featured, MAARS provided parallel results across the age and sex subgroups, which is a key aspect of equity in healthcare.
Interpretability: MAARS is also not a black box. It describes the reason that it makes a prediction using such techniques as Shapley values of clinical data and attention rollout of images. As an example, it found things such as non sustained ventricular tachycardia, high scar burden (LGE%) and non obstructive HCM to be more risky and an even higher maximum exercise heart rate target and particular in echocardiogram result to be less risky. This enables physicians to recognize and believe in the rationale of the AI and obtain new clinical information.
Management of Imbalance: SCDA incidents are not frequent. This challenge did not affect the capabilities of MAARS to differentiate high-risk patients.
The importance of this: The future of HCM care
The consequences are far reaching:
Individualized Safeguard: MAARS will find it much easier to distinguish the genuinely “high-risk” HCM patients who are in urgent need of preventive ICDs that are now losing their lives through sudden death.
Elimination of unnecessary procedures: On the other hand, it can also help to establish that low risk individuals can be spared of the risks and burdensome aspects of an unnecessary implant of ICD.
Blazing the Trail: MAARS interpretability might be applicable in the treatment of targeted therapies more than ICDs alone.
A Template to Medicine: MAARS shows how the combination of multiple types and forms of medical data, particularly raw imaging, with the application of advanced AI can solve difficult clinical prediction tasks and offers a template to the application of similar tools in other diseases.
Issues and the Future
There are no breakthroughs without restrictions. Supplementary validation of MAARS must be done in still larger, more varied groups, and with greater longitudinal follow-up. The next practical requirement is to seamlessly integrate its analysis into clinical workflows, which may be necessitated by automated data extraction. The amount of computational capacity required is within the range of feasibility (~0.1 seconds per prediction per patient) and thus infrastructure is required.
Conclusion: A Data Driven and Brighter Future
MAARS marks a gigantic step in controlling the horrific possibility of sudden death in hypertrophic cardiomyopathy. It has been able through the use of multimodal AI and deep learning applied to a full dataset of patient information, including the wealth of information contained within raw cardiac MRI scans, to produce a prediction of arrhythmic death risk with a fairness and interpretability previously unachievable. Though it needs more validation, MAARS seems like a lighthouse, showing how artificial intelligence can bring us to the distant shore of genuinely personalized and, more importantly, life-saving care in patients with HCM. The future of cardiac risk assessment is in its smart, networked, and breathtaking future.
Reference
Original Study in Nature Cardiovascular Research
Lai, C., Yin, M. et al. “Multimodal AI to forecast arrhythmic death in hypertrophic cardiomyopathy.” Nat Cardiovasc Res (2025).